Insurance will cover a maximum of four cycles of ovulation induction three cycles of intrauterine insemination IUI two cycles of IVF GIFT ZIFT or low tubal ovum transfer with no more than two embryo implantations per cycle. Anthem Blue Cross Blue Shield of GA PPO POS HMO.
 Costs Coverage Issues Spur Black Market For Fertility Meds
Costs Coverage Issues Spur Black Market For Fertility Meds
Insurance coverage for fertility treatments like IVF can get extremely complicated.
What insurance covers ivf in georgia. CCRM Atlanta is out-of-network with all Anthem BCBS plans. All individual group and blanket health insurance policies that provide for medical or hospital expenses shall include coverage for fertility care services including IVF and standard fertility preservation services for individuals who must undergo medically necessary treatment that may cause iatrogenic infertility. Armed services and TriCare for active military personnel and their families.
Such benefits must be provided to the same extent as other pregnancy-related benefits and. The IVF cost in Georgia can range between 10000 to 13000 excluding medication and testing. Insurance is Aetna POS.
Digit Health Insurance covers Accidental Illness COVID-19 Hospitalization Pin Code healthCtrlresidentPincodeError close. Infertility testing and diagnosis are generally covered while fertility treatments such as IVF and egg freezing are not reimbursed by insurance. For IVF services BCBSA gives coverage to members if only specified in the member contract.
The Blue Cross Blue Shield Association BCBSA stands out as one of the most recognized insurance providers in the US. Non-profit insurance companies Blue CrossBlue Shield plans. Commercial insurance Aetna Cigna United.
Delaware requires that infertility treatment be covered to the same degree as pregnancy-related benefits. It covers all testing and unlimited IUI no IVF or FET. The average cost of IVF Medication is between 2500 and 5000.
Georgia is one of the states that do not enjoy the benefits of insurance. United Healthcare is our overall pick for fertility insurance because of its expansive network solid reputation and coverage for infertility services including ovulation induction insemination and. Whether or not you have coverage it is important to understand what costs are associated with your treatment and what options you have for funding.
Will cover all types of infertility 5000 limit per year 10000 maximum. 23-79-510 specifies that the Arkansas Comprehensive Health Insurance Pool shall not include coverage for any expense or charge for in vitro fertilization artificial insemination or any other artificial means used to cause pregnancy. Below youll find a list of all posts that have been tagged as what insurance covers ivf in georgia What is the Cost of Male Infertility Treatment in Georgia 2021.
The company covers all aspects of healthcare including infertility treatments such as IVF and IUI for its policyholders. In Georgia like many states coverage for fertility testing and treatment is based on insurance carriers and individual plans. Some employers have elected to cover the cost of fertility.
Must have four month history of ttc. All IF tx including IVF BlueCross Blue Shield of Georgia. The term infertility describes the incapability of a couple to achieve conception in spite of repeated attempts of trying.
Contact IVF1s insurance coverage professionals to schedule a consultation by clicking below or calling 6303576540. The resulting embryos are transplanted to your uterus. Eggs are gathered from your ovaries and combined with your spouses sperm in a laboratory dish.
2000 copay each visit. These decisions are usually made by the Human Resources Department before the open enrollment period every year. Is fertility testing and treatment covered by insurance plans in the state of Georgia.
Aetna - PPO POS EPO MC HMO and Indemnity Institute of Excellence designation by Aetna since 2008. 3 GIFT Gamete Intrafallopian Transfer. Kaiser Permanente Insurance Coverage for IVF FAQ.
Private insurance falls into one of three categories. In order to access those services your employer must opt-in to infertility coverage for their plan members explains Tablada. Why We Chose It.
Depending on your state employer and coverage plan you may or may not have benefits in terms of financing your fertility care. Patients with these plans will be self-pay. This monthly grant covers CNYs 3900 IVF cycle which includes retrieval anesthesia ICSI assisted hatching one transfer cryopreservation and storage for one year.
23-85-137 and 23-86-118 1987 2011. Email submission 1903 Agency Mortgage Corporation. Yes Kaiser patients who have IVF benefits will need to have an authorization from their Kaiser physician.
Meds covered but must be pre-certified-no copay. Do you accept Kaiser Permanente insurance for fertility treatment. If your insurance plan doesnt have fertility coverage speak with your HR department about getting the coverage added to your companys insurance.
IVF In Virto Fertilisation. Nearly all insurance plans have the ability to cover infertility treatment. Medication monitoring and other services are not included.
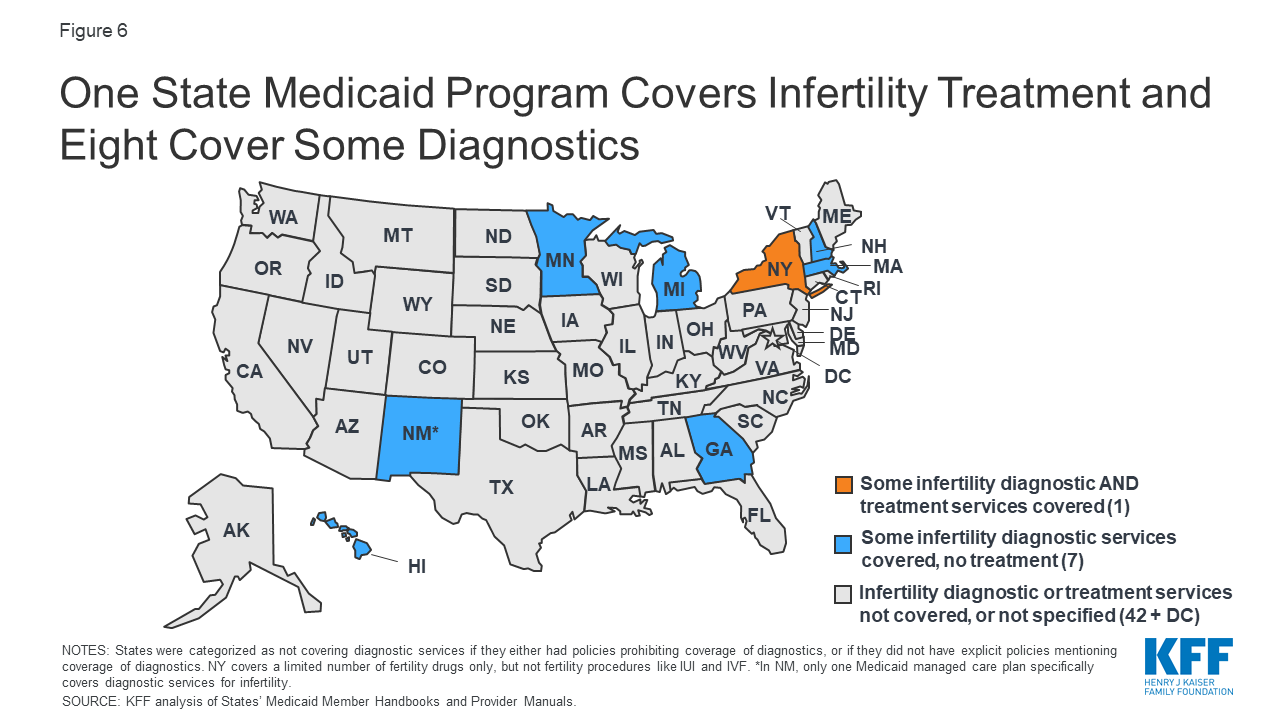
Public insurance includes government policies such as Medicaid for the poor Medicare for the elderly or disabled Veterans Administration for the US. Your eggs are removed mixed. State Laws Related to Infertility Treatments.
The insurance experts at IVF1 will make certain that your insurance policys benefits are maximized as a financial source to cover your infertility treatment.
